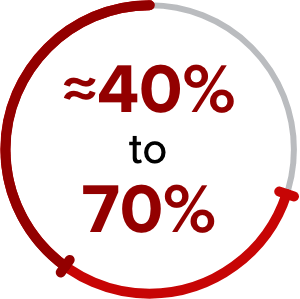
of patients ended JAK inhibition therapy within 3 years of treatment initiation due to intolerance, loss of response, or disease progression4†
Current patient care commonly focuses on SYMPTOMS1-3
Management strategies:
- Low- and intermediate-1 risk: Watch and wait; anemia-directed therapy; other symptom-directed therapy based on the clinical situation1
- Intermediate-2 and high-risk: JAK inhibition; ASCT (for select patients)5
- Current guidelines recommend ASCT only for eligible patients who are predicted to have poor survival based on prognostic risk scores (IPSS, DIPSS, and DIPSS Plus)6
- In a retrospective study, 3% of MF patients received ASCT7*
- Low- and intermediate-1-risk patients are not routinely offered ASCT6
What causes MF progression?9-12
Progressive bone marrow fibrosis can lead to continued symptoms and is associated with poor outcomes13,14
- Symptom persistence: Inflammatory cytokine production leads to constitutional symptoms10-13
- Patient impact: BMF-related anemia at diagnosis has been associated with inferior quality of life and poor outcomes; it may also limit patient treatment eligibility13,15
*Retrospective study conducted by a single institution.7
†In a 24-week, placebo-controlled trial, 54.1% of patients with MF did not see an improvement of 50% or more in total symptom score at 24 weeks, even if they experienced reduced symptom burden (N=309).16
‡Based on analyses of 2 large US claims databases, IMS Health® and MarketScan®.8
ASCT=allogeneic stem cell transplantation; BMF=bone marrow fibrosis; DIPSS=Dynamic International Prognostic Scoring System; IPSS=International Prognostic Scoring System; JAK=Janus kinase; JAK/STAT=Janus kinase signal transducer and activator of transcription; MF=myelofibrosis.
References:
- Harrison CN, Schaap N, Mesa RA. Management of myelofibrosis after ruxolitinib failure. Ann Hematol. 2020;99:1177-1191. doi:10.1007/s00277-020-04002-9
- Newberry KJ, Patel K, Masarova L, et al. Clonal evolution and outcomes in myelofibrosis after ruxolitinib discontinuation. Blood. 2017;130(9):1125-1131. doi:10.1182/blood-2017-05-783225
- Ross DM, Babon JJ, Tvorogov D, Thomas D. Persistence of myelofibrosis treated with ruxolitinib: biology and clinical implications. Haematologica. 2021;106(5):1244-1253. doi:10.3324/haematol.2020.262691
- Kuykendall AT, Shah S, Talati C. Between a rux and a hard place: evaluating salvage treatment and outcomes in myelofibrosis after ruxolitinib discontinuation. Ann Hematol. 2018;97:435-441. doi:10.1007/s00277-017-3194-4
- Schieber M, Crispino JD, Stein B. Myelofibrosis in 2019: moving beyond JAK2 inhibition. Blood Cancer J. 2019;9(9):74. doi:10.1038/s41408-019-0236-2
- Devlin R, Gupta V. Myelofibrosis: to transplant or not to transplant? Hematology Am Soc Hematol Educ Program. 2016;2016(1):543-551. doi:10.1182/asheducation-2016.1.543
- Tefferi A, Lasho TL, Jimma T, et al. One thousand patients with primary myelofibrosis: the Mayo Clinic experience. Mayo Clin Proc. 2012;87(1):25-33. doi:10.1016/j.mayocp.2011.11.00
- Fonseca E, Silver RT, Kazis LE, Iqbal SU, Rose M, Khan N. Ruxolitinib discontinuation in patients with myelofibrosis: an analysis from clinical practice. Blood. 2013;112(21):2833. doi:10.1182/blood.V122.21.2833.2833
- Kramann R, Schneider RK. The identification of fibrosis-driving myofibroblast precursors reveals new therapeutic avenues in myelofibrosis. Blood. 2018;131(19):2111-2119. doi:10.1182/blood-2018-02-834820
- Gleitz HFE, Pritchard JE, Kramann R, Schneider RK. Fibrosis driving myofibroblast precursors in MPN and new therapeutic pathways. HemaSphere. 2019;3(S2):142-145. doi:10.1097/HS9.0000000000000216
- Gleitz HFE, Kramann R, Schneider RK. Understanding deregulated cellular and molecular dynamics in the haematopoietic stem cell niche to develop novel therapeutics for bone marrow fibrosis. J Pathol. 2018;245(2):138-146. doi:0.1002/path.5078
- Agarwal A, Morrone K, Bartenstein M, et al. Bone marrow fibrosis in primary myelofibrosis: pathogenic mechanisms and the role of TGF-β. Stem Cell lnvestig. 2016;3:5. doi:10.3978/j.issn.2306-9759.2016.02.03
- Zahr AA, Salama ME, Carreau N, et al. Bone marrow fibrosis in myelofibrosis: pathogenesis, prognosis and targeted strategies. Haematologica. 2016;101(6):660-671. doi:10.3324/haematol.2015.141283
- Nazha A, Estrov Z, Cortes J, Bueso-Ramos CE, Kantarjian H, Verstovsek S. Prognostic implications and clinical characteristics associated with bone marrow fibrosis in patients with myelofibrosis. Leuk Lymphoma. 2013;54(11):2537-2539. doi:10.3109/10428194.2013.769537
- Naymagon L, Mascarenhas J. Myelofibrosis-related anemia: current and emerging therapeutic strategies. HemaSphere. 2017;1(1):e1. doi:10.1097/HS9.0000000000000001
- Verstovsek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799-807. doi:10.1056/NEJMoa1110557