Sustained reduction of spleen volume
Further exploration is needed to uncover solutions that are able to control BOTH THE SYMPTOMS AND THE UNDERLYING DISEASE1,2
Current and potential future goals for managing myelofibrosis could include1-6:
In a US MPN Landmark survey, the most important treatment goal for patients with myelofibrosis was to slow or delay disease progression7
- Other important goals for patients included better quality of life, healthy blood counts, and symptom improvement7
A closer look at some potential management goals:
Sustained reduction of spleen volume
JAK inhibition typically achieves SVR ≥35% in ≈40% of patients at 24 weeks8,9
The majority may not sustain SVR10
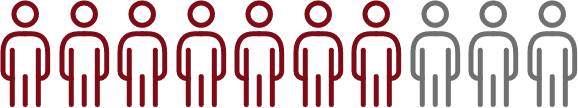
≈70% did not sustain SVR at ≈3 years
(Landmark clinical trial)10
≈70% did not sustain SVR at
≈3 years (Landmark clinical trial)10
Anemia response for longer transfusion-free periods
All patients with MF are at risk of developing anemia3
At diagnosis, nearly 40% of patients with MF have hemoglobin (Hb) levels <10 g/dL and nearly one-quarter are already RBC transfusion dependent3

In some patients, durable anemia response could help mitigate symptoms or allow for longer transfusion-free periods, improving quality of life3,11
Reversal of bone marrow fibrosis
BMF is a key diagnostic feature (2008 WHO criteria) of MF12
In a long-term follow-up study, reduced BMF* with JAK inhibition was correlated with:
Targeting the malignant stem cell may disrupt the downstream signaling that contributes to BMF2,5,14
The heterogeneity of treatment experiences, durations, and response definitions continues to pose clinical challenges19
AbbVie is committed to ongoing research in myelofibrosis.
*Measured by grade of reticulin and collagen deposition.13
BMF=bone marrow fibrosis; IWG-MRT=International Working Group-Myeloproliferative Neoplasms Research and Treatment; JAK=Janus kinase; JAK/STAT=Janus kinase signal transducer and activator of transcription; MF=myelofibrosis; MPN=myeloproliferative neoplasm; RBC=red blood cells; SVR=spleen volume reduction; WHO=World Health Organization.
References:
- Pettit K, Odenike O. Novel therapies for myelofibrosis. Curr Hematol Malig Rep. 2017;12(6):611-624. doi:10.1007/s11899-017-0403-0
- Schieber M, Crispino JD, Stein B. Myelofibrosis in 2019: moving beyond JAK2 inhibition. Blood Cancer J. 2019;9(9):74. doi:10.1038/s41408-019-0236-2
- Naymagon L, Mascarenhas J. Myelofibrosis-related anemia: current and emerging therapeutic strategies. HemaSphere. 2017;1(1):e1. doi:10.1097/HS9.0000000000000001
- Tefferi A, Guglielmelli P, Pardanani A, Vannucchi AM. Myelofibrosis treatment algorithm 2018. Blood Cancer J. 2018;8(8):72. doi:10.1038/s41408-018-0109-0
- Kramann R, Schneider RK. The identification of fibrosis-driving myofibroblast precursors reveals new therapeutic avenues in myelofibrosis. Blood. 2018;131(19):2111-2119. doi:10.1182/blood-2018-02-834820
- Tefferi A, Lasho TL, Jimma T, et al. One thousand patients with primary myelofibrosis: the Mayo Clinic experience. Mayo Clin Proc. 2012;87(1):25-33. doi:10.1016/j.mayocp.2011.11.001
- Mesa RA, Miller CB, Thyne M, et al. Myeloproliferative neoplasms (MPNs) have a significant impact on patients’ overall health and productivity: the MPN Landmark survey. BMC Cancer. 2016;16:167. doi:10.1186/s12885-016-2208-2
- Verstovsek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799-807. doi:10.1056/NEJMoa1110557
- Pardanani A, Harrison C, Cortes JE, et al. Safety and efficacy of fedratinib in patients with primary or secondary myelofibrosis: a randomized clinical trial. JAMA Oncol. 2015;1(5):643-651. doi:10.1001/jamaoncol.2015.1590
- Verstovsek S, Mesa RA, Gotlib J, et al. Long-term treatment with ruxolitinib for patients with myelofibrosis: 5-year update from the randomized, double-blind, placebo-controlled, phase 3 COMFORT-I trial. J Hematol Oncol. 2017;10(1):55. doi:10.1186/s13045-017-0417-z
- Mughal TI, Vaddi K, Sarlis NJ, Verstovsek S. Myelofibrosis-associated complications: pathogenesis, clinical manifestations, and effects on outcomes. Int J Gen Med. 2014;7:89-101. doi:10.2147/IJGM.S51800
- Zahr AA, Salama ME, Carreau N, et al. Bone marrow fibrosis in myelofibrosis: pathogenesis, prognosis and targeted strategies. Haematologica. 2016;101(6):660-671. doi:10.3324/haematol.2015.141283
- Kvasnicka HM, Thiele J, Bueso-Ramos CE. Long-term effects of ruxolitinib versus best available therapy on bone marrow fibrosis in patients with myelofibrosis. J Hematol. 2018;11(1):42. doi:10.1186/s13045-018-0585-5
- Santos FPS, Verstovsek S. Therapy with JAK2 inhibitors for myeloproliferative neoplasms. Hematol Oncol Clin North Am. 2012;26(5):1083-1099. doi:10.1016/j.hoc.2012.07.008
- Vannuchi AM, Pieri L, Guglielmelli P. JAK2 allele burden in the myeloproliferative neoplasms: effects on phenotype, prognosis and change with treatment. Ther Adv Hematol. 2011;2(1):21-32. doi:10.1177/2040620710394474
- Hasselbalch HC. The role of cytokines in the initiation and progression of myelofibrosis. Cytokine Growth Factor Rev. 2013;24(2):133-145. doi:10.1016/j.cytogfr.2013.01.004
- Pemmaraju N, Verstovsek S, Mesa R, et al. Defining disease modification in myelofibrosis in the era of targeted therapy. Cancer. 2022;128(13):2420-2432. doi:10.1002/cncr.34205
- Harrison CN, McLornan DP. Current treatment algorithm for the management of patients with myelofibrosis, JAK inhibitors, and beyond. Hematology Am Soc Hematol Educ Program. 2017;(1):489-497. doi:10.1182/asheducation-2017.1.489
- Harrison CN, Schaap N, Mesa RA. Management of myelofibrosis after ruxolitinib failure. Ann Hematol. 2020;99:1177-1191. doi:10.1007/s00277-020-04002-9
- Tefferi A, Cervantes F, Mesa R, et al. Revised response criteria for myelofibrosis: International Working Group-Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) and European LeukemiaNet (ELN) consensus report. Blood. 2013;122(8):1395-1398. doi:10.1182/blood-2013-03-488098
- Rubert J, Qian Z, Andraos R, Guthy DA, Radimerski T. Bim and Mcl-1 exert key roles in regulating JAK2V617F cell survival. BMC Cancer. 2011;11:24. doi:10.1186/1471-2407-11-24
- Tremblay D, Mascarenhas J. Next generation therapeutics for the treatment of myelofibrosis. Cells. 2021;10(5):1034. doi:10.3390/cells10051034